

SUMMARY
It is sometimes difficult to assess our images quickly and efficiently without forgetting some important area of error. Here is a quick easy checklist to assess your images for repeat.








WHAT MUST WE SEE IN THE MLO PROJECTION?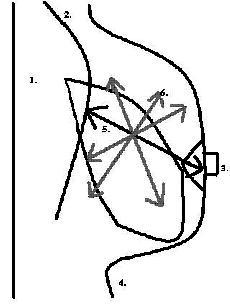
HOW DO WE MEASURE THE PECTORALIS?
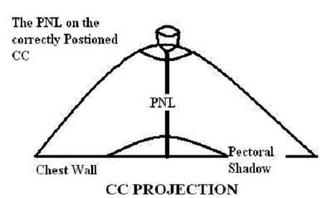
We draw a line parallel to the Cooper’s ligaments from the nipple base to the pectoral shadow or the film edge which ever comes first; where the PNL intersects with the Pectoral shadow shows us if we are above the nipple, at the nipple or below the nipple.

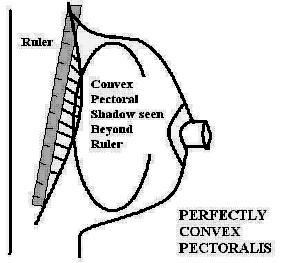
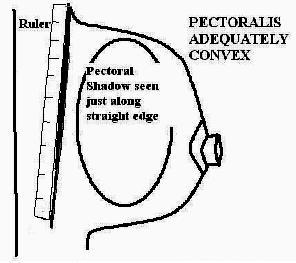
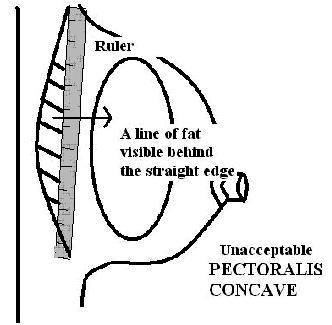
To calculate the convex nature of the pectoral shadow, hold a straight edge from the top outer aspect of the pectoral to the bottom corner. If there is muscle showing in front of the ruler, the shadow is convex. If there is breast tissue or fat showing behind the ruler the muscle is concave.
WHEN IS PECTORAL MUSCLE CONCAVE?
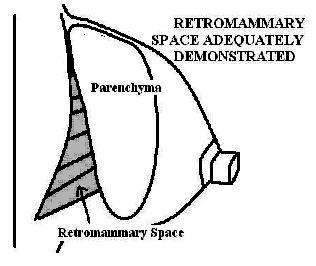
WHEN IS THE RETRO-MAMMARY SPACE SEEN?
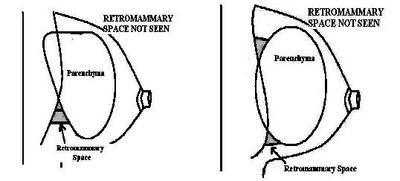
If the retro mammary space is not demonstrated behind the parenchyma on the MLO view we have not seen all the breast tissue that is at risk. To avoid missing breast cancers we must understand when the tissue is adequately seen and when it is not and extra images are called for.
WHEN IS THE RETRO-MAMMARY SPACE NOT SEEN?
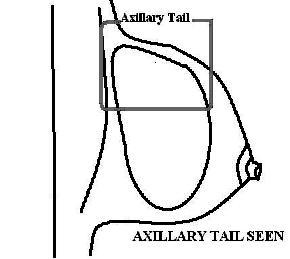
WHEN IS THE AXILLARY TAIL FULLY DEMONSTATED?
To ensure the axillary tail is adequately seen on the MLO projection, the tail-of-Spence should be clearly visible at the superior border of the image. There should be a line of retro mammary fat above the superior parenchymal edge. A gently curving edge of tissue should be visible leading up toward the axilla.
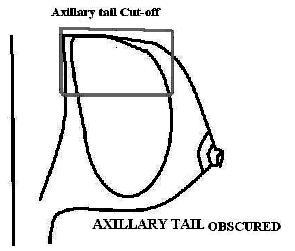
WHEN IS THE AXILLARY TAIL NOT FULLY DEMONSTATED?
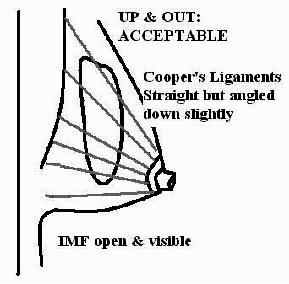
WHEN IS THE BREAST ‘UP & OUT’?
If the breast is perfectly up and out in the oblique view the pattern of the cooper’s ligaments should be perpendicular to the chest wall. If the cooper’s ligaments are at least straight from the nipple base back to the chest wall, the up and out position of the breast is adequate.
Breast In Perfect ‘Up & Out’ Position:
Breast Adequately ‘Up & Out’:
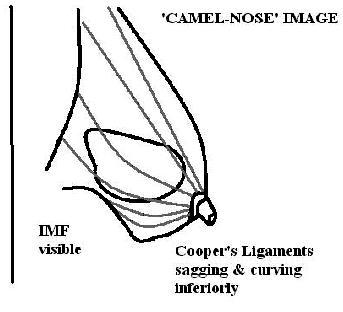
WHEN IS THE BREAST NOT ‘UP & OUT’?
Breast NOT ‘Up & Out’:
Breast In ‘Camel nose’ NOT ‘Up & Out’:
WHEN IS THE IMF OPEN AND ADEQUATELY VISUALIZED?
This is the most common error made by technologists when assessing their images for accreditation or certification submission. Many of us misinterpret a large fold of abdomen imaged at the back of the breast as inframammary fold. A bright light will help determine what we are observing at the inferior aspect of our images.
The true IMF will be grey, like fat and skin. It will appear as a gentle curve beyond and below the parenchyma. Again, a hot light will tell us for sure that we are seeing IMF and not a big fold or wrinkle surrounded by air.
IMF Open and Clearly Demonstrated
IMF Open and Seen Just Above a fold of Abdomen BELOW the Level of the Breast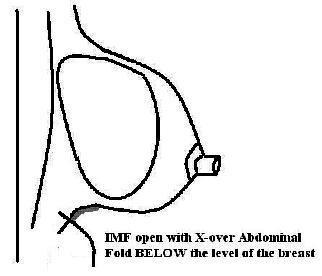
WHEN IS THE IMF NOT OPEN AND ADEQUATELY VISUALIZED?
Summary:
Our mission as mammographers gets more complicated every year. We are called upon to assess patients, images, equipment and services. Breast imaging is complex but not beyond skills. Everything follows certain recognized standards, adhere to these and things will not seem so demanding.
WHEN DO WE SEE THE MEDIAL CROSS-OVER?
WHEN DON'T WE SEE THE MEDIAL CROSS-OVER?
WHEN DON'T WE SEE THE NIPPLE IN PROFILE?
WHEN DO WE SEE RETRO MAMMARY SPACE?
Adequately Demonstrated Pectoralis
WHEN DON'T WE SEE PECTORAL SHADOW?

MEASURING THE POSTERIOR NIPPLE LINE
The PNL on the CC projection is ALWAYS measured from the base of the nipple directly back to the film edge. The measurement is taken this way irregardless of pectoralis shadow or improper positioning.
Our mission as mammographers gets more complicated every year. We are called upon to assess patients, images, equipment and services. Breast imaging is complex but not beyond skills. Everything follows certain recognized standards, adhere to these and things will not seem so demanding.
Mammonewsline is updated periodically, publishing articles of interest to mammographers and other diagnostic imaging technologists. I'm always looking for column ideas, and I love getting your questions and comments, so feel free to contact me.